A Trojan Horse Explanation of the SARS-CoV-2 Attack
A collaborative piece of research published in July on eLife, done by scientists from various centers in Connecticut, Kentucky, Ohio, Tennessee, and Wisconsin, has stirred up the conversion about Covid-19. It presented a a sort of unified hypothesis about SARS-CoV-2 that can explain many of its seemingly psychotic behaviors and point to clinical interventions that are already on the market.
The title of the paper is “A mechanistic model and therapeutic interventions for COVID-19 involving a RAS-mediated bradykinin storm.” It is rather obscure for the lay person, and it certainly doesn’t sound revolutionary. But those who understand have described it as so. Why?
While it is only the tip of the iceberg in terms of Covid-19 research, this work brings together various previously disjointed pieces of knowledge and offers a rather astonishing view of the Covid-19 landscape. And, just as the tip of an iceberg, it sits on a huge amount of previous works that made possible this very visible one.
Using what they learnt from the previous research, the scientists loaded their data onto a supercomputer called Summit to run 2.5 billion correlation calculations on thousands of samples from Covid-19 patients and controls (people not infected). By the way, it took Summit abut a week to run those calculations.
Setting the Scene
I will try to summarize its content without any of the complex biochemistry that it refers to.
To do this, I will tell you the story of SARS-CoV-2 as a mole in “Trojan Horse.” By now, we have all heard that the virus has spiky proteins that it uses to attach itself to the host’s cells. The host is us, by the way, the people that the virus infects.
Its protein spikes happen to fit right into ACE2 receptors’ nooks, like a lock and key situation. ACE2 is the Trojan Horse that ushers the virus into the body. (The virus also attaches to another receptor, but we’ll stick to one here.) ACE2 or angiotensin converting enzyme 2 is a protein involved in a vital biochemical pathway that regulates processes such as blood pressure, wound healing, and inflammation. This pathway is called RAAS, for Renin-Angiotensin-Aldosterone System (also called RAS).
The Characters
The RAAS pathway is one of the characters in the unfolding of the Covid-19 story. It consists of a cascade of enzymatic processes that balance vasoconstriction and vasodilation (narrowing and opening of the blood vessels) as well as blood viscosity, thereby adjusting blood pressure.
The fact the the virus messes with blood pressure is one reason why people with hypertension and cardiac conditions are at higher risk: the virus imposes greater burden on a system already stressed.
Normally, the narrowing of blood vessels is controlled by the Vasoconstrictive ACE Axis of the RAAS system. What an ominous name, right? But this axis or arm, as some call it, basically involves two hormones, renin and angiotensin-converting-enzyme or ACE that trigger a series of protein transformations to ultimately yield Angiotensin 2 (Ang2). Ang2 binds to receptors in the cells (called AT1), and that binding prompts a sort of compactor mechanism with a constricting effect, that is, it closes up the vessels (not completely, of course) and thus elevates blood pressure.
The balance to this narrowing mechanism is the equally ominous Vasorelaxant ACE2 Counter Axis. This axis has anti-hypertensive properties, it lowers blood pressure. The bigger angiotensin 2 is broken down (by hydrolysis or water fracturing) into angiotensin 1-7 and 1-9. These smaller compounds bind with different receptors and trigger a vasodilating effect, similarly to how the release mechanism of the compactor opens it up.
Two other characters are important in this Trojan horse story: bradykinin and hyaluronic acid. Bradykinin is a small protein (a peptide hormone) that dilutes blood viscosity (by preventing the clumping of platelets in the blood) and opens up blood vessels (by relaxing smooth muscles). This is not done by bradykinin alone but by a series of compounds that bradykinin orchestrates, including prostacyclin, which you may have heard is used for pulmonary hypertension.
Bradykinin, like other kinins, increases vascular permeability and is involved in pain perception. The result of its dilution and permeability powers is a decrease in blood pressure. Another interesting effect is that it induces thirst in mammals.
Now, let’s introduce the last character, hyaluronic acid or HA. Many will know it as a skin care humectant used for its ability to draw and hold water. Indeed, in the body, it is a polymer (or large molecule) that can absorb more than 1,000 times its weight in water! HA plays a lubricating role throughout the body; its production increases during injury to promote wound healing and has a role in activating inflammatory cells to enhance immune response.
This is all under normal circumstances. Now, let’s see what happens when SARS-CoV-2 infects the body.
The Villain: SARS-CoV-2
SARS-CoV-2 enters cells in a Trojan horse fashion by hitching a ride on ACE2 receptors. Once inside the body, the virus causes the levels of ACE in the lung cells to decrease and the levels of ACE2 to increase.
Early studies interpreted the chaos in the RAAS system balance as viral slashing of ACE-2 and ramping of ACE, resulting in higher blood pressure, vasoconstriction, inflammation, and cell damage. But, the research mentioned above actually found a far more sophisticated set of events.
To start, SARS-CoV-2 can survive the extreme pH of the gastrointestinal (GI) tract. Upon spreading into the body, the virus delivers a series of devastating blows.
The First Blow: Suppressing ACE
When the virus comes face to face with cells that in principle should launch an immune response against the invader, SARS-CoV-2 does something quite clever: in another Trojan horse-like move, it repurposes the cell guards, a protein called interferon, for its own protection. It does so by stealing the shielding power from interferon. A casualty in this battle is a messenger of intelligence called NFkappaB activating factor. This messenger usually prompts production of ACE for vasoconstriction (to narrow blood vessels). The virus slashes ACE production 10-fold. The virus acts, in effect, as a blood pressure lowering medication.
The Second Blow: Ramping up ACE2
The production shutdown of ACE (technically called downregulation) tips off the RAAS balance. While the ACE Axis is suppressed, the ACE2 Counter Axis is ramped up (upregulated). Remember that SARS-CoV-2 uses ACE2 as its Trojan horse, so it makes sense (for the virus) to replicate ACE2. In fact, the increase has been estimated at almost 200-fold!
The imbalance of a suppressed ACE Axis and a rampant ACE2 Counter Axis results in more bradykinin being produced due to lack of ACE and more Ang1-9 being produced due to excess ACE2. Both of these compounds, bradykinin and Ang1-9 intensify vasodilation, inflammatory pain, and vascular permeability—or leaky blood vessel walls.
The Third Blow: Hyaluronic Invasion
Simultaneously, the virus messes with the production of hyaluronic acid or HA. The genes involved in HA synthesis are encouraged to overproduce and the genes that direct HA degradation are almost brought to a halt. The result of these two shifts is an accumulation of HA in the lungs.
As you know, the lungs are a pair of spongy, air-filled organs. The air is housed in the alveoli, which are tiny permeable balloons that bring oxygen to the bloodstream. When excess HA in the alveoli “absorbs” the fluid now dripping from leaky blood vessels, the alveoli turn not just into water balloons but Jell-O-filled balloons that are no longer permeable. In Figure 1, the research team illustrated the closing of this air exchange border. This causes the dry cough we heard so much about in covid-19 patients: they are literally gasping for air.
Figure 1: Formation of a HA-hydrogel that inhibits gas exchange in the alveoli of COVID-19 patients.
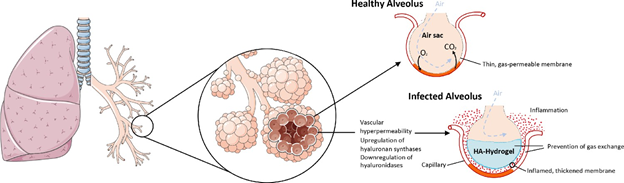
Source: https://elifesciences.org/articles/59177#s2
The Bradykinin Storm Turns into a Category Five Hurricane
These series of small changes caused by SARS-CoV-2 conflate to create a worst case scenario, where the overdrive of mechanisms for lowering blood pressure creates leaky blood vessels and the overproduction of a lubricating substance creates a gel pool that drowns the cells and processes around it.
The research paper had another illustrative visual, shown in Figure 2.
Figure2: Systemic-level effects of critically imbalanced RAAS and BK pathways.
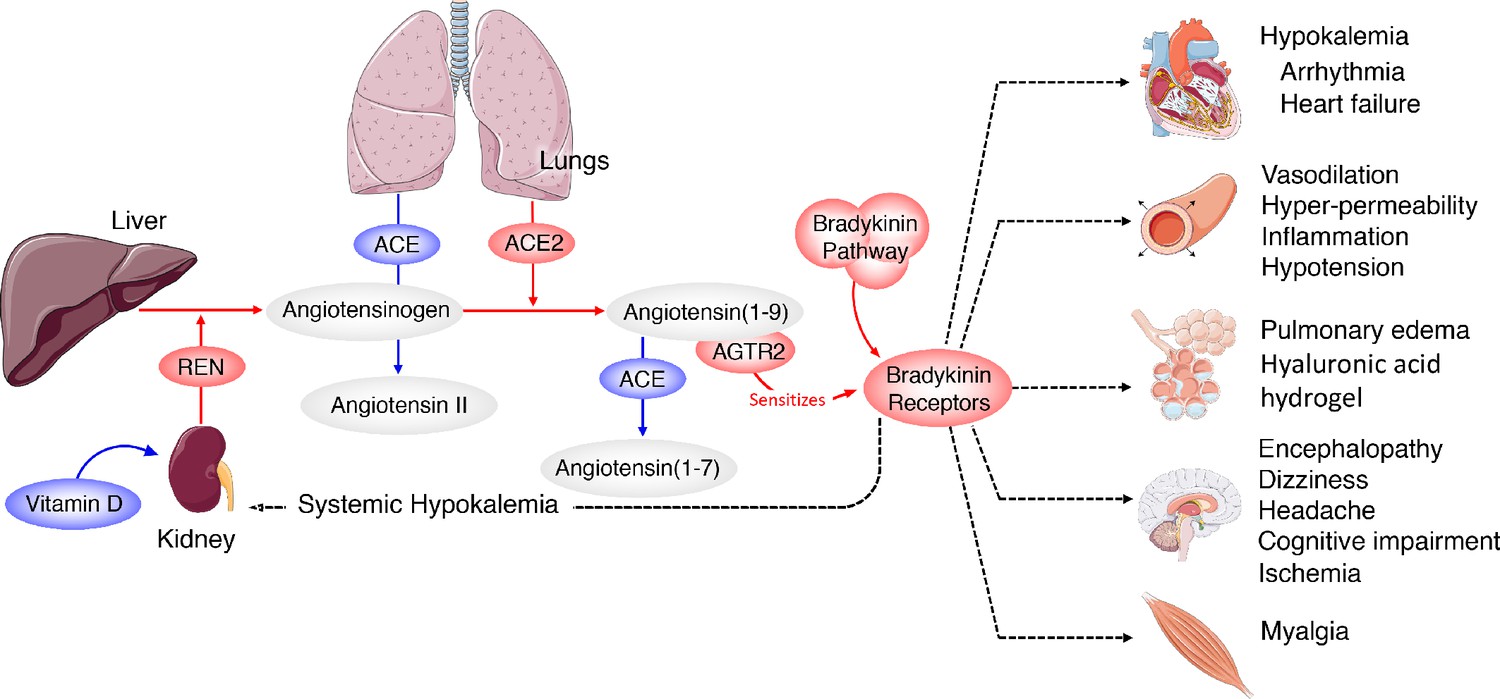
Source: https://elifesciences.org/articles/59177#s2
Rebuilding
While the research was focused on understanding the mechanisms of Covid-19 infection, it also points to clinical interventions to explore, particularly those already available on the market for increasing ACE, decreasing BK, or blocking BK2 receptors (which, as their name indicates help BK run amok during the infection).
Another suggestion points to the control of renin levels (the R in the RAAS pathway) through Vitamin D supplementation. Vitamin D promotes calcium absorption in the gut and maintains the balance of other minerals. Through its role in mineral balance, Vitamin D also has a strong supporting role in the balance of the RAAS pathway. The medications suggested for these interventions are presented in table 1.
The published paper of course emphasizes the importance of testing these interventions through well-designed clinical trials. The paper closes with a great suggestion: “Given the likely future outbreaks of zoonotic viruses [originating in animals] with a similar outcome, it would be in the best interest long-term to invest in the development of small molecules that can inhibit the virus from replicating or suppressing the host immune system […]. In the meantime, our analyses suggest that prevention and treatment centered on vascular hyper-permeability and the suppression of hyaluronan [the precursor to HA] may prove beneficial in fighting the pathogenesis of COVID-19.”
Table 1: Potential therapeutic interventions, their targets, and predicted effect.
| Drug | Target | Predicted Effect |
| Danazol, Stanozolol | SERPING1 | Reduce Bradykinin production |
| Icatibant | BKB2R | Reduce Bradykinin signaling |
| Ecallantide | KLKB1 | Reduce Bradykinin production |
| Berinert,Cinryze,Haegarda | SERPING1 | Reduce Bradykinin production |
| Vitamin D | REN | Reduce Renin production |
| Hymecromone | HAS1,HAS2, HAS3 | Reduce hyaluronan |
Source: https://elifesciences.org/articles/59177#s2
